With the 2015 healthcare marketplace open enrollment concluded, more and more patients are finding they can’t see their long-standing physicians with the new insurance plans. To control costs, many Affordable Care Act (ACA) plans, particularly at the Bronze and Silver levels, featured narrow provider networks last year, and the trend has continued this year.
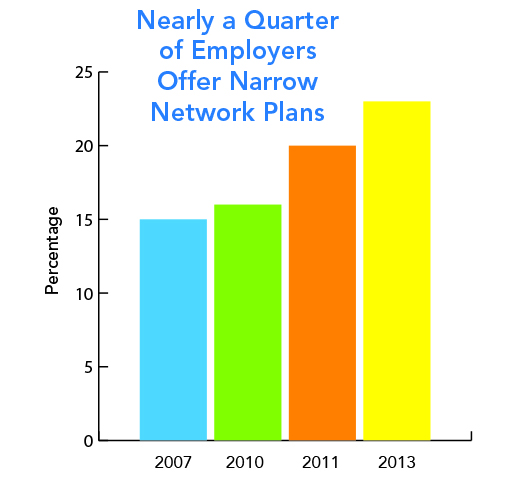
Commercial plans have also started to take this approach, offering the reduced-choice options as high performing (and lower cost) networks to major employers. With 56% of insured Americans obtaining coverage through their employers, this could potentially affect millions of patients and hundreds of thousands of physicians.
Insurers have used narrow networks as a strategy to reduce premiums. As a result insurance companies are dropping physicians from Medicare Advantage networks without notice or explanation. Incredibly, docs seem to be getting the bad rap rather than insurers. Physicians are being blamed for charging excessively high rates or refusing to negotiate with insurers.
The challenges of getting into networks may increase in the short term as hospitals and integrated healthcare systems, such as the Mayo Clinic, Cleveland Clinic, Massachusetts General Hospital/Partners, and others create their own HMOs. These healthcare systems have a clear financial incentive to create narrow networks to keep patients and reimbursements within the system.
Based on a survey conducted by the Medical Group Management Association.
