- Endoscopic retrograde cholangiopancreatography (ERCP) is not cost effective for treatment of borderline common bile duct stones (CBDS).
- Conservative management of CBDS is associated with decreased length of hospital stay, fewer complications, and reduced cost.
- Conservative management of CBDS obviates the surgical challenges associated with ERCP for borderline cholelethiasis.
- Conservative management is equally effective as ERCP for removal of borderline common bile duct stones.
- Post-ERCP pancreatitis occurred significantly more frequently in patients in the ERCP group.
The results of a small prospective, randomized study published recently in the Journal of Laparoendoscopic & Advanced Surgical Techniques suggest that conservative management of borderline common bile duct with stones is both more cost effective and clinically superior to more aggressive management with endoscopic retrograde cholangiopancreatography (ERCP).

The Study
“Management of common bile duct stones (CBDS) in patients with borderline CBD presents a surgical challenge. The aim of this study was to compare conservative treatment with endoscopic stone extraction for the treatment of borderline CBD with stones,” the authors explained.
The prospective randomized controlled trial included patients with CBDS in borderline CBD (CBD <10 mm) associated with gallbladder stones. Patients underwent treatment with either a conservative approach or endoscopic stone extraction followed by laparoscopic cholecystectomy (LC) and intraoperative cholangiogram (IOC).
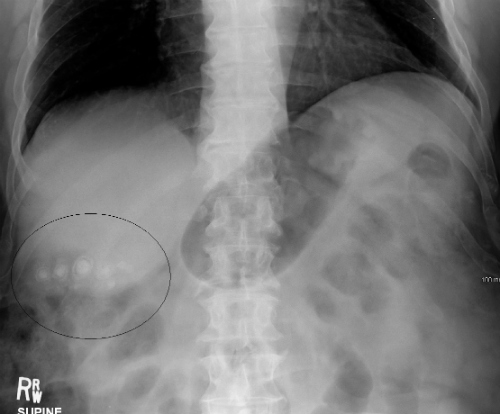
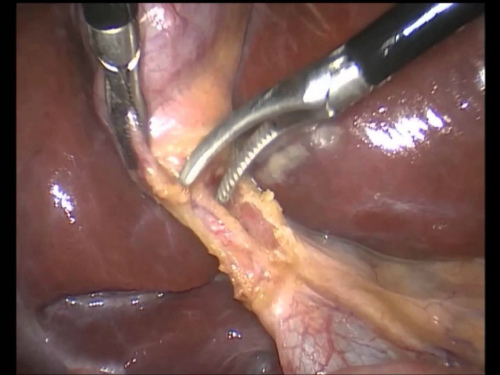
LC and IOC resulted in complete clearance of CBDS in 48 (96%) cases in the ERCP (Figure 2) group. Among these patients, 52% had stones cleared by ERCP, and 44% were able to pass the stone spontaneously. In the remaining 2 patients, the CBDS was removed by transcystic exploration.

In the group of patients who underwent conservative treatment, LC (Figure 4) and IOC resulted in complete clearance of CBDS in 90% of cases, and in the remaining 10% of patients, the CBDS (Figure 3) were removed by transcystic exploration. Post-ERCP pancreatitis (PEP) occurred significantly more frequently in the ERCP group (2 [4%] versus 8 [16%]; P=0.04).
The average net cost was significantly higher in the ERCP group and recurrent biliary symptoms developed significantly more frequently in the ERCP group at 1-year follow up (10% versus 0%; P=0.02). These symptoms were recurrent cholangititis and recurrent CBDS.
“Management of CBDS in patients with borderline CBD represents a surgical challenge. Borderline CBD increases the technical difficulty of ERCP and increases the risk of PEP. Conservative management of CBDS in borderline CBD not only avoids the risks inherent in ERCP and unnecessary preoperative ERCP, but it is also effective in clearing CBDS. The hepatobiliary surgeon should consider a conservative line of treatment in CBDS in borderline CBD in order to decrease the cost and avoid unnecessary ERCP,” the authors concluded.
